42 Sleep Problems and Disorders
Learning Objectives
By the end of this section, you will be able to:
- Describe the symptoms and treatments of insomnia
- Recognize the symptoms of several parasomnias
- Describe the symptoms and treatments for sleep apnea
- Describe the symptoms and treatments for narcolepsy
Many people experience disturbances in their sleep at some point in their lives. Depending on the population and sleep disorder being studied, between 30% and 50% of the population suffers from a sleep disorder at some point in their lives (Bixler, Kales, Soldatos, Kaels, & Healey, 1979; Hossain & Shapiro, 2002; Ohayon, 1997, 2002; Ohayon & Roth, 2002). This section will describe several sleep disorders as well as some of their treatment options.
Insomnia
Insomnia, a consistent difficulty in falling or staying asleep, is the most common of the sleep disorders. Individuals with insomnia often experience long delays between the times that they go to bed and actually fall asleep. In addition, these individuals may wake up several times during the night only to find that they have difficulty getting back to sleep. As mentioned earlier, one of the criteria for insomnia involves experiencing these symptoms for at least three nights a week for at least one month’s time (Roth, 2007).
It is not uncommon for people suffering from insomnia to experience increased levels of anxiety about their inability to fall asleep. This becomes a self-perpetuating cycle because increased anxiety leads to increased arousal, and higher levels of arousal make the prospect of falling asleep even more unlikely. Chronic insomnia is almost always associated with feeling overtired and may be associated with symptoms of depression.
There may be many factors that contribute to insomnia, including age, drug use, exercise, mental status, and bedtime routines. Not surprisingly, insomnia treatment may take one of several different approaches. People who suffer from insomnia might limit their use of stimulant drugs (such as caffeine) or increase their amount of physical exercise during the day. Some people might turn to over-the-counter (OTC) or prescribed sleep medications to help them sleep, but this should be done sparingly because many sleep medications result in dependence and alter the nature of the sleep cycle, and they can increase insomnia over time. Those who continue to have insomnia, particularly if it affects their quality of life, should seek professional treatment.
Some forms of psychotherapy, such as cognitive-behavioural therapy, can help sufferers of insomnia. Cognitive-behavioural therapy is a type of psychotherapy that focuses on cognitive processes and problem behaviours. The treatment of insomnia likely would include stress management techniques and changes in problematic behaviours that could contribute to insomnia (e.g., spending more waking time in bed). Cognitive-behavioural therapy has been demonstrated to be quite effective in treating insomnia (Savard, Simard, Ivers, & Morin, 2005; Williams, Roth, Vatthauer, & McCrae, 2013).
Parasomnias
A parasomnia is one of a group of sleep disorders in which unwanted, disruptive motor activity and/or experiences during sleep play a role. Parasomnias can occur in either REM or NREM phases of sleep. Sleepwalking, restless leg syndrome, and night terrors are all examples of parasomnias (Mahowald & Schenck, 2000).
Sleepwalking
In sleepwalking, or somnambulism, the sleeper engages in relatively complex behaviours ranging from wandering about to driving an automobile. During periods of sleepwalking, sleepers often have their eyes open, but they are not responsive to attempts to communicate with them. Sleepwalking most often occurs during slow-wave sleep, but it can occur at any time during a sleep period in some affected individuals (Mahowald & Schenck, 2000).
Historically, somnambulism has been treated with a variety of pharmacotherapies ranging from benzodiazepines to antidepressants. However, the success rate of such treatments is questionable. Guilleminault et al. (2005) found that sleepwalking was not alleviated with the use of benzodiazepines. However, all of their somnambulistic patients who also suffered from sleep-related breathing problems showed a marked decrease in sleepwalking when their breathing problems were effectively treated.
REM Sleep Behaviour Disorder (RBD)
REM sleep behaviour disorder (RBD) occurs when the muscle paralysis associated with the REM sleep phase does not occur. Individuals who suffer from RBD have high levels of physical activity during REM sleep, especially during disturbing dreams. These behaviours vary widely, but they can include kicking, punching, scratching, yelling, and behaving like an animal that has been frightened or attacked. People who suffer from this disorder can injure themselves or their sleeping partners when engaging in these behaviours. Furthermore, these types of behaviours ultimately disrupt sleep, although affected individuals have no memories that these behaviours have occurred (Arnulf, 2012).
This disorder is associated with a number of neurodegenerative diseases such as Parkinson’s disease. In fact, this relationship is so robust that some view the presence of RBD as a potential aid in the diagnosis and treatment of a number of neurodegenerative diseases (Ferini-Strambi, 2011). Clonazepam, an anti-anxiety medication with sedative properties, is most often used to treat RBD. It is administered alone or in conjunction with doses of melatonin (the hormone secreted by the pineal gland). As part of treatment, the sleeping environment is often modified to make it a safer place for those suffering from RBD (Zangini, Calandra-Buonaura, Grimaldi, & Cortelli, 2011).
Other Parasomnias
A person with restless leg syndrome has uncomfortable sensations in the legs during periods of inactivity or when trying to fall asleep. This discomfort is relieved by deliberately moving the legs, which, not surprisingly, contributes to difficulty in falling or staying asleep. Restless leg syndrome is quite common and has been associated with a number of other medical diagnoses, such as chronic kidney disease and diabetes (Mahowald & Schenck, 2000). There are a variety of drugs that treat restless leg syndrome: benzodiazepines, opiates, and anticonvulsants (Restless Legs Syndrome Foundation, n.d.).
Night terrors result in a sense of panic in the sufferer and are often accompanied by screams and attempts to escape from the immediate environment (Mahowald & Schenck, 2000). Although individuals suffering from night terrors appear to be awake, they generally have no memories of the events that occurred, and attempts to console them are ineffective. Typically, individuals suffering from night terrors will fall back asleep again within a short time. Night terrors apparently occur during the NREM phase of sleep (Provini, Tinuper, Bisulli, & Lagaresi, 2011). Generally, treatment for night terrors is unnecessary unless there is some underlying medical or psychological condition that is contributing to the night terrors (Mayo Clinic, n.d.).
Sleep Apnea
Sleep apnea is defined by episodes during which a sleeper’s breathing stops. These episodes can last 10–20 seconds or longer and often are associated with brief periods of arousal. While individuals suffering from sleep apnea may not be aware of these repeated disruptions in sleep, they do experience increased levels of fatigue. Many individuals diagnosed with sleep apnea first seek treatment because their sleeping partners indicate that they snore loudly and/or stop breathing for extended periods of time while sleeping (Henry & Rosenthal, 2013). Sleep apnea is much more common in overweight people and is often associated with loud snoring. Surprisingly, sleep apnea may exacerbate cardiovascular disease (Sánchez-de-la-Torre, Campos-Rodriguez, & Barbé, 2012). While sleep apnea is less common in thin people, anyone, regardless of their weight, who snores loudly or gasps for air while sleeping, should be checked for sleep apnea.
While people are often unaware of their sleep apnea, they are keenly aware of some of the adverse consequences of insufficient sleep. Consider a patient who believed that as a result of his sleep apnea he “had three car accidents in six weeks. They were ALL my fault. Two of them I didn’t even know I was involved in until afterwards” (Henry & Rosenthal, 2013, p. 52). It is not uncommon for people suffering from undiagnosed or untreated sleep apnea to fear that their careers will be affected by the lack of sleep, illustrated by this statement from another patient, “I’m in a job where there’s a premium on being mentally alert. I was really sleepy… and having trouble concentrating…. It was getting to the point where it was kind of scary” (Henry & Rosenthal, 2013, p. 52).
There are two types of sleep apnea: obstructive sleep apnea and central sleep apnea. Obstructive sleep apnea occurs when an individual’s airway becomes blocked during sleep, and air is prevented from entering the lungs. In central sleep apnea, disruption in signals sent from the brain that regulate breathing cause periods of interrupted breathing (White, 2005).
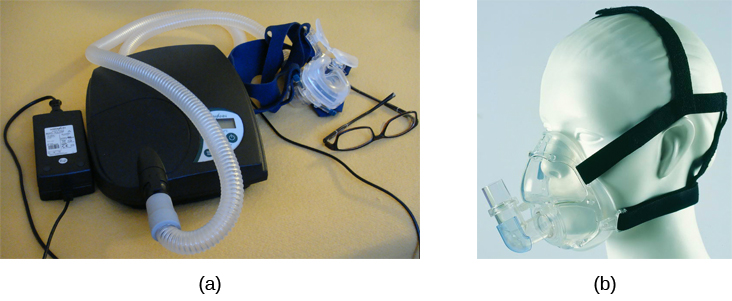
One of the most common treatments for sleep apnea involves the use of a special device during sleep. A continuous positive airway pressure (CPAP) device includes a mask that fits over the sleeper’s nose and mouth, which is connected to a pump that pumps air into the person’s airways, forcing them to remain open, as shown in Figure SC.14. Some newer CPAP masks are smaller and cover only the nose. This treatment option has proven to be effective for people suffering from mild to severe cases of sleep apnea (McDaid et al., 2009). However, alternative treatment options are being explored because consistent compliance by users of CPAP devices is a problem. Recently, a new EPAP (expiratory positive air pressure) device has shown promise in double-blind trials as one such alternative (Berry, Kryger, & Massie, 2011).
Narcolepsy
Unlike the other sleep disorders described in this section, a person with narcolepsy cannot resist falling asleep at inopportune times. These sleep episodes are often associated with cataplexy, which is a lack of muscle tone or muscle weakness, and in some cases involves complete paralysis of the voluntary muscles. This is similar to the kind of paralysis experienced by healthy individuals during REM sleep (Burgess & Scammell, 2012; Hishikawa & Shimizu, 1995; Luppi et al., 2011). Narcoleptic episodes take on other features of REM sleep. For example, around one third of individuals diagnosed with narcolepsy experience vivid, dream-like hallucinations during narcoleptic attacks (Chokroverty, 2010).
Surprisingly, narcoleptic episodes are often triggered by states of heightened arousal or stress. The typical episode can last from around a minute to half an hour. Once awakened from a narcoleptic attack, people report that they feel refreshed (Chokroverty, 2010). Obviously, regular narcoleptic episodes could interfere with the ability to perform one’s job or complete schoolwork, and in some situations, narcolepsy can result in significant harm and injury (e.g., driving a car or operating machinery or other potentially dangerous equipment).
Generally, narcolepsy is treated using psychomotor stimulant drugs, such as amphetamines (Mignot, 2012). These drugs promote increased levels of neural activity. Narcolepsy is associated with reduced levels of the signalling molecule hypocretin in some areas of the brain (De la Herrán-Arita & Drucker-Colín, 2012; Han, 2012), and the traditional stimulant drugs do not have direct effects on this system. Therefore, it is quite likely that new medications that are developed to treat narcolepsy will be designed to target the hypocretin system.
There is a tremendous amount of variability among sufferers, both in terms of how symptoms of narcolepsy manifest and the effectiveness of currently available treatment options. This is illustrated by McCarty’s (2010) case study of a 50-year-old woman who sought help for the excessive sleepiness during normal waking hours that she had experienced for several years. She indicated that she had fallen asleep at inappropriate or dangerous times, including while eating, while socializing with friends, and while driving her car. During periods of emotional arousal, the woman complained that she felt some weakness in the right side of her body. Although she did not experience any dream-like hallucinations, she was diagnosed with narcolepsy as a result of sleep testing. In her case, the fact that her cataplexy was confined to the right side of her body was quite unusual. Early attempts to treat her condition with a stimulant drug alone were unsuccessful. However, when a stimulant drug was used in conjunction with a popular antidepressant, her condition improved dramatically.

